March 2016
Bone marrow transplantation and gene therapy as a treatment for leukodystrophies
In this article the process of bone marrow transplant and gene therapy will be first explained, before describing the applications and results obtained in leukodystrophies.
The aim of a bone marrow transplant is to replace the cells of the bone marrow and blood of a patient with those taken from a healthy person. The aim of gene therapy is to repair a patient’s deficient cells by introducing a normal version of the gene involved in the disease. There are possibilities to repair a gene, in the true meaning of the word, (in particular with the CRISPR/Cas9 technique), but they are not yet used in the clinic.
Bone marrow transplantation
“Allogeneic” bone marrow transplant meaning, from a donor, involves replacing the deficient bone marrow cells of a patient with those of a healthy donor.
Bone marrow and hematopoietic stem cells
The bone marrow is a diffuse organ located inside the bones. It is a factory in which billions of cellular elements of blood are made, where they are born and multiply. Three major cell families circulate in the blood: red blood cells responsible for oxygen transport, white blood cells (polynuclear cells, lymphocytes and monocytes) providing defenses against infections, and platelets responsible for preventing bleeding by activating coagulation.
The bone marrow makes these different elements from special cells, called hematopoietic stem cells. These cells, called undifferentiated, are like a canvas that can be used to make what the body needs. These cells are able to multiply and differentiate into red blood cells, white blood cells or platelets. Red blood cells and platelets have a relatively long half-life (120 days for red blood cells and 10 days for platelets). Plynuclea cells and monocytes, in contrast, have a shorter half-life and renew rapidly. If needed, the reserve is mobilized, and the production of cells is intensified. The bone marrow is essential to life.
Differents steps
- The different sources of hematopoietic stem cells: stem cells are present in the marrow, peripheral blood or in the umbilical cord of newborns, also called placental blood.
- The choice of donor: the donor can be an unaffected brother or sister with an identical tissue compatibility complex (HLA system). It can be an unrelated, anonymous donor sought from national and international registries. The current chances, given the existence of 13 million donors worldwide, are 40-50% to find a compatible donor for a patient waiting for transplant. There are also cord blood registries that increase the probability to find a compatible donor to at least 80%.
- Sample of the donor: in the case of a bone marrow donation, the sample is collected by bone punctures of the iliac crests (pelvic bone) of the donor under general anesthesia, removing a sufficient quantity of cells for normal recovery of the recipient after transplant. The quantity required is in the order of 10 ml/kg of body weight of the receiver.
When sample is from peripheral blood cells, it is necessary to use a drug (a hematopoietic growth factor) to allow stem cells from the bone marrow to move into the peripheral blood, where they can be sampled by cytapheresis and then separated. Cytapheresis is based on the principle that blood cells do not have the same weight and can therefore be separated by centrifugation. The pretreatment with a growth factor can cause bone pain to the donor and a headache, that will quickly disappear when treatment is stopped. - Placental blood is the blood of the newborn. Naturally, newborn blood contains a fairly large quantity of hematopoietic stem cells. However, some of the newborn blood (on the placenta side) is not used by the newborn and can therefore be taken just after the birth of the child and serve as a hematopoietic stem cell graft. The fact is that placental blood is an overall more tolerant graft than a bone marrow one. Then placental blood grafts that are not totally HLA identical to the patient can be used. This is very important because it will allow to transplant patients who need a transplant but do not have an identical HLA donor, from a sibling, or from the different registries of bone marrow volunteer donors. The difficulty of this type of transplantation is the relatively small quantity of cells injected that causes longer aplasia times and explains the initial indication in small children. Solutions are being developed either by manipulation of the graft or by the use of 2 grafts.
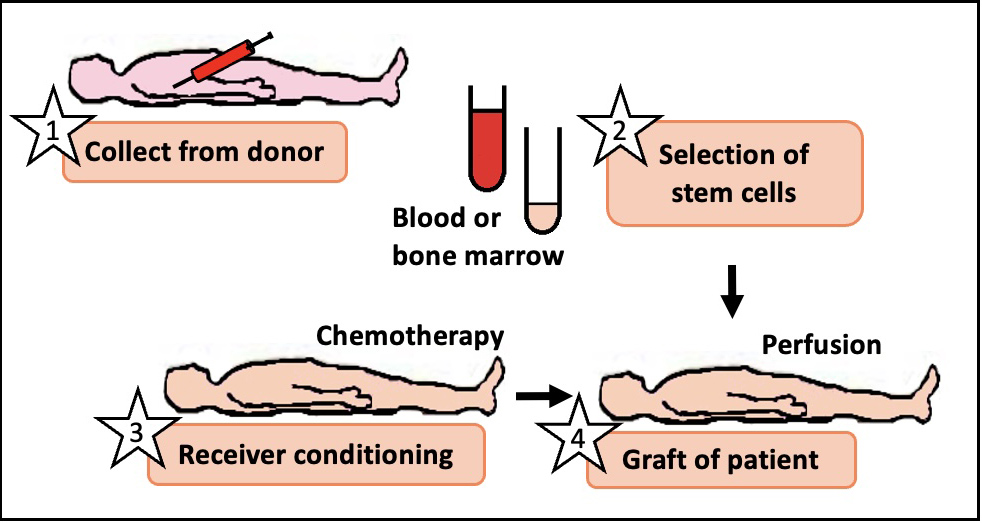
Stapes of bone marrow transplant
- Conditioning of the recipient: before the patient can receive the donor cells, the patient’s sick medullary cells must be destroyed by chemotherapy. The adverse effects are digestive disorders (nausea, vomiting, diarrhea), ulcerations of the oral cavity, temporary hair loss. Treatments are provided to prevent and treat these effects.
- The transfer of the graft consists for the recipient in a simple transfusion of stem cells. The injected cells will circulate and then settle in the bone marrow. The two weeks following the perfusion are delicate, because the patient no longer has stem cells and can no longer make blood cells, in particular the new white blood cells needed to defend himself against infections, and the platelets needed to prevent bleeding; and this until the stem cells from the donor reproduce. Aseptic precautions (sterile room) are then essential. It is a difficult time to pass through, physically because the patient is tired, and psychologically because the wait is long and agonizing.
Complications.
As with any transplant, even with a compatible donor, the risk of rejection exists. The patient’s immune cells that remain in the organs, including lymphocytes, may attack the graft (rejection), as well as the graft cells may attack the patient (graft versus host disease). These complications can sometimes lead to death.
For all these reasons, the development of alternative treatments to bone marrow transplantation is desirable. In this sense, gene therapy, if made possible, appears as an interesting alternative solution. By using the patient’s own cells, the risk of rejection and of graft versus disease host are avoided.
Results of clinical trials of bone marrow transplant for leukodystrophies
Between 1999 and 2011, 152 studies have been published worldwide, describing bone marrow transplant trials in 689 patients with leukodystrophy (adrenoleukodystrophy, metachromatic leukodystrophy and Krabbe diseases). Results indicate the benefit of bone marrow transplant in patients with few or no symptoms.
Indeed, a retrospective study conducted in 2007 shows that the 5-year survival of patients with cerebral adrenoleukodystrophy who have received a bone marrow transplant is close to 95%, compared to only 54% in patients who have not been transplanted. Five years later, symptoms are stable in 53% of transplanted patients, compared to only 6% of patients without transplants.
However, treatment is not beneficial for patients who have already developed more severe symptoms. Bone marrow transplantation is recommended for patients with few or no symptoms and with a compatible donor.
Gene therapy
Some technical notions
Gene therapy involves repairing a patient’s deficient cells. To repair cells, two methods are possible:
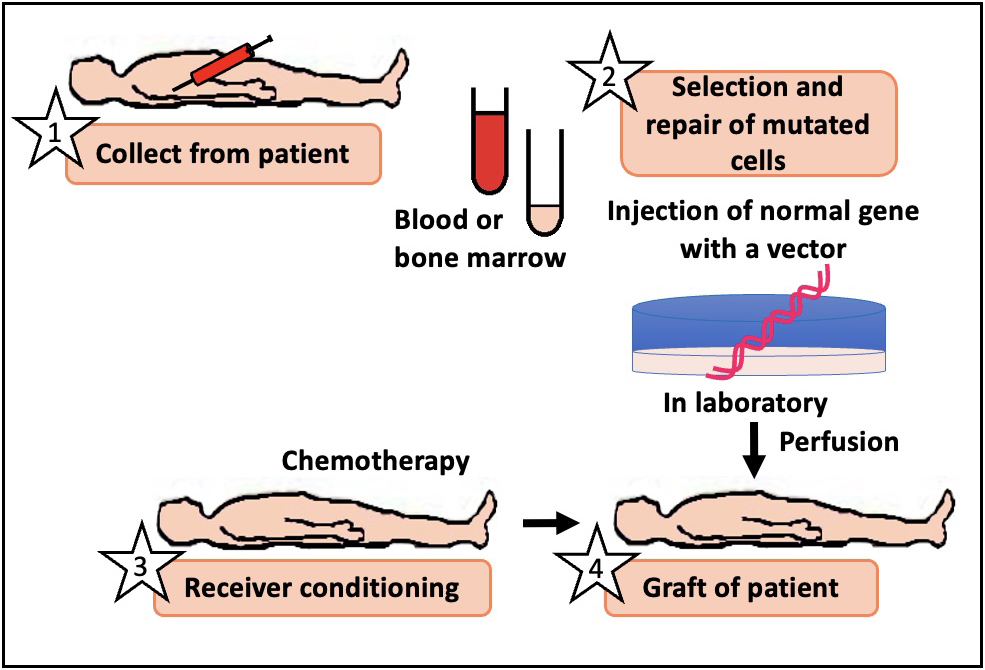
Stapes of gene therapy
- either hematopoietic stem cells are collected from the patient: they are repaired in the laboratory by adding a healthy copy of the gene responsible for the disease and the corrected cells are reinjected into the patient, after the same chemotherapy as for a bone marrow transplant with a donor is done: this is called ex vivo gene therapy based on hematopoietic stem cell transplant
- either a viral vector is injected (today most often an AAV, a small non-pathogenic DNA virus) directly into the blood or brain of the patient and will enter into the diseased cells of the brain and repair those cells by adding a normal version of the gene in question: this is called in vivo gene therapy.
Gene therapy vectors
They are viruses. We still have not found a better solution for the moment. We use their ability to “infect” (penetrate) cells with genetic material. But the genetic material of the virus is replaced by the gene of the disease to be treated. These viruses cannot multiply and spread. They are called “non-infectious”. There are two main types of gene therapy viral vectors used today. Lentiviral vectors, used for gene therapy of hematopoietic stem cells, which allow to put the therapeutic gene in chromosomes, in the middle of other genes. AAV vectors that allow the therapeutic gene to be placed in the form of a DNA circle (as is the case with the genetic material of bacteria) in the cell nucleus. In the first case, the therapeutic gene is transmitted to all the daughter cells of the corrected cells, if they divide, and to all the cells derived from them. In the second case, the therapeutic gene is transmitted to only 50% of the daughter cells, and if the corrected cells divide much, the therapeutic gene ends up being lost.
Application for Leukodystrophies
Gene therapy for hematopoietic stem cells is limited to only three leukodystrophies: adrenoleukodystrophy (ALD), metachromatic leukodystrophy (MLD) and possibly Krabbe disease. After hematopoietic stem cell transplantation and bone marrow reconstruction, a sub-population of specialized cells will move to the brain and become microglial cells. In the case of metachromatic leukodystrophy and Krabbe disease, microglial cells will produce the normal lysosomal enzyme (ARSA in metachromatic leukodystrophy, and GALC in Krabbe disease). The enzyme produced can be recaptured by other uncorrected cells, especially oligodendrocytes. Adrenoleukodystrophy is not due to the deficit of an enzyme, but to the deficit of a protein that remains in the cells and participates in the degradation of very long chain fatty acids.
In adrenoleukodystrophy, hematopoietic stem cell transplantation from a donor or hematopoietic stem cell gene therapy only repairs microglial brain cells, not oligodendrocytes. However, this is enough to stop the brain demyelination process.
For all other leukodystrophies, it is necessary to put the therapeutic gene directly in the cells of the brain: oligodendrocytes, astrocytes or both. So a gene therapy vector that is able to penetrate those cells is needed, whether the vector is injected directly into the brain or intravenously. For some forms of leukodystrophy (like Pelizaeus-Merzbacher disease due to duplications of the PLP gene, or Alexander disease due to mutations of the GFAP gene that give the diseased cells a new function), it is not necessary to put a copy of the normal gene but to introduce genetic material (derived from an RNA most often) that can decrease the mutated gene expression level.
The choice of vectors and the method of administration
The choice of vectors used to carry the therapeutic gene depends on the type of cells to be corrected and therefore the type of leukodystrophy.
In the case of gene therapy using bone marrow stem cells, there is no other choice than to use lentivirus. But the therapeutic gene is placed anywhere in the chromosomes, anywhere in other genes. Then there is a risk to disturb the normal growth cycle of bone marrow cells and to induce leukemia with other additional factors. However, no such complication has been observed so far in more than 30 treated patients. The vector must be able to carry a large therapeutic gene, if the gene of the disease is large. This is the case for lentivirus, but not for AAV vectors. When injected intravenously, the gene therapy vector must be able to pass the blood-brain barrier to reach the brain. This is the case for some types of AAV, but not all AAV, and lentivirus do not pass the blood-brain barrier, or very poorly. The vector can be injected directly into the brain or even into the cerebrospinal fluid (as for a lumbar puncture). But the diffusion of vectors from injection/penetration sites into brain tissue is low, which requires multiple intra-cerebral injections. This increases the risk of causing an intracerebral hematoma.
For intravenous and intrathecal injections (in cerebrospinal fluid), it is necessary to determine the quantity of virus to be injected, to check that the virus is not toxic to other organs, because it is necessary to inject very large quantity of virus.
The blood-brain barrier
Because it is so important to the functioning of the body overall, the brain is well protected. It bathes in a liquid and is encapsulated in the skull. Blood-cell contact is close in all organs. But the brain is an exception. There is a barrier that controls entry and exit such as a customs post. It is the blood-brain barrier, formed of cells from brain vessels, astrocytes and specialized cells called pericytes. And while it is there to protect the brain, this barrier also limits access of treatments developed by doctors. In the case of intravenous gene therapy applied to leukodystrophies, the passage of the blood-brain barrier represents a major challenge. Researchers are working to modify the envelope of viruses to allow them to pass this blood-brain barrier.
Results of clinical trials of gene therapy for leukodystrophies
A total of 42 children (21 ALD, 20 MLD, 13 Canavan disease) participated in gene therapy clinical trials.
- In Adrenoleukodystrophie (ALD)
The first trials of gene therapy in adrenoleukodystrophy, largely funded by ELA, were conducted by the team of Pr. Aubourg in four patients with a cerebral adrenoleukodystrophy and with no available compatible donor. They showed that the therapy was feasible and well tolerated. Indeed, for the first time in the world, hematopoietic stem cells collected from patients with cerebral adrenoleukodystrophy were modified ex-vivo to correct the genetic defect causing the disease, before being re-injected into the patients. This innovative approach of gene therapy stopped the progression of the disease 14 to 16 months after injection, in 3 of the 4 patients treated, with similar results for efficiency as bone marrow transplant of hematopoietic stem cells. This gene therapy treatment is actually tested (Phase II/III) in 17 other patients and will be extended to other children. As with the hematopoietic stem cell transplant using a donor, it can only be offered to patients with adrenoleukodystrophy presenting no symptom of the cerebral form of the disease, and having no compatible sibling permitting a bone marrow transplant.
- In metachromatic leukodystrophy (MLD)
Clinical trials of gene therapy were conducted by the team of Dr. Biffi in Italy on 20 patients with metachromatic leukodystrophy. They showed that the treatment was well tolerated by the patients. The first results also show that clinical benefit is possible for patients treated at the pre-symptomatic stage, several months before the first motor symptoms appear. It is not clear yet if there is an efficiency in patients with symptom, same as after a hematopoietic stem cell transplant. This is probably because the disease progresses too quickly and that it takes at least 12 months before a sufficient number of corrected microglial cells are obtained to have a clinical effect.
- In Canavan desease
No relevant therapeutic benefits were obtained. However, we must say that this old trial was conducted with a low-performing type of AAV vector that is no longer used and that the treated patients had a very advanced form of their disease.
Conclusions
With more than twenty-five years of hindsight, the results indicate a benefit of marrow transplant in patients with adrenoleukodystrophy, in children with late form of metachromatic leukodystrophy (called «juvenile» forms) and Krabbe disease when transplant is done at birth for early forms or in late forms of the disease. In all cases, the results indicate that the transplant has no effect in children with manifest symptoms of the disease. It only works at the very beginning of the disease, in practice mainly when patients do not yet have clear symptoms.
Perspectives
Gene therapy trials in patients with adrenoleukodystrophy and metachromatic leukodystrophy are very hopeful. But these treatments only concern children treated at the very beginning of their disease or better without symptoms. A gene therapy trial, funded by ELA is in progress in metachromatic leukodystrophy (Pr. Aubourg), using intracerebral injection of AAV vector. For Krabbe disease, studies are still at the preclinical stage, in mouse, dog or monkey. For all other leukodystrophies, a specific strategy of gene therapy will have to be developed. The gene therapy will not be a treatment for all leukodystrophies.
The first steps towards gene therapy in the treatment of leukodystrophies could be implemented in large part thanks to donations made to ELA to support research against leukodystrophies.



